Background: Red blood cell (RBC) transfusions are often used to treat patients with iron deficiency who present to the emergency department (ED) with symptomatic anemia. Intravenous (IV) iron is the preferred treatment in this setting, as it has been shown to increase hemoglobin concentration rapidly and durably. We aim to determine the incidence of iron deficiency anemia (IDA) and the management of these patients in the ED setting.
Objectives: To evaluate the incidence of IDA, the frequency of RBC transfusion and iron supplementation, and factors associated with RBC transfusion.
Study Design: Retrospective cohort study of all adult patients presenting to the St Boniface Hospital (Winnipeg, CAN) ED from January 2014 to January 2019.
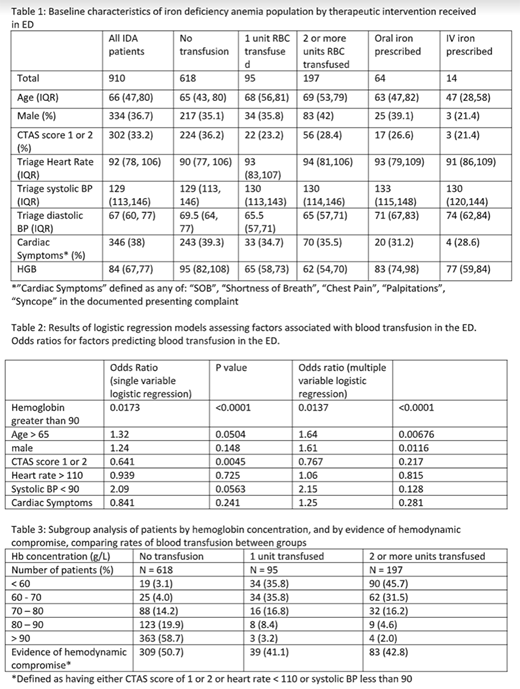
Methods: We used electronic data from the Emergency Department Information System (EDIS) and Laboratory Information Services (LIS) databases to identify patients presenting with IDA, defined as anemia (hemoglobin <120 g/L) with either a transferrin saturation less than 20% or ferritin less than 30 umol/L, or mean corpuscular volume (MCV) of < 75 fL. A ferritin greater than 100 umol was used to exclude IDA, regardless of MCV. We extracted patient demographics, diagnoses, markers of iron storage, RBC transfusion and use of IV iron. Multivariate logistic regression analysis was used to evaluate factors associated with RBC transfusion.
Results: Of 39222 patients, 17945 (45%) were anemic. Of the anemic patients, iron parameters were ordered in 1848 (10.3%) patients, and IDA was present in 910 (5.1 %). In the IDA population, 95 patients (10.4 %) received 1 RBC unit, and 197 patients (21.6 %) received 2 or more units. Oral iron and IV iron were prescribed for 64 (7 %) and 14 (1.5 %) patients, respectively. Our logistic regression model demonstrated that hemoglobin concentration was the main determinant of whether patients received RBC transfusion. Other variables including patient age, cardiac symptoms, heart rate, blood pressure, and CTAS score were not associated with increased likelihood of receiving RBC transfusion.
Conclusion: Iron parameters were infrequently ordered in the evaluation of anemia in the ED, with limited use of oral and IV iron. The decision to transfuse RBCs was primarily influenced by hemoglobin concentration, but not other surrogates of hemodynamic instability. An interventional study to improve education and access to oral and IV iron is planned to reduce unnecessary RBC transfusions and their associated risks in patients with IDA.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal